Drug Catalog - Product Detail
TUBERSOL INJ SOL 5T/0.1ML 10T X 1ML
| NDC | Mfr | Size | Str | Form |
|---|---|---|---|---|
| 49281-0752-21 | SANOFI PASTEUR | 1 | 5UNIT/0.1ML | SOLUTION |
PACKAGE FILES
Generic Name
TUBERCULIN PURIFIED PROTEIN DERIVATIVE
Substance Name
TUBERCULIN PURIFIED PROTEIN DERIVATIVE
Product Type
HUMAN PRESCRIPTION DRUG
Route
INTRADERMAL
Application Number
BLA103941
Description
DESCRIPTION TUBERSOL ® Tuberculin Purified Protein Derivative (Mantoux) (PPD) (1) for intradermal tuberculin testing is prepared from a large Master Batch Connaught Tuberculin (CT68) (2) and is a cell-free purified protein fraction obtained from a human strain of Mycobacterium tuberculosis grown on a protein-free synthetic medium and inactivated. (2) The use of a standard preparation derived from a single batch (CT68) has been adopted in order to eliminate batch to batch variation by the same manufacturer. (2) TUBERSOL is a clear, colorless liquid. TUBERSOL contains: Purified protein derivative of M. tuberculosis 5 TU per 0.1 mL Polysorbate 80 0.0006% Phenol 0.22% to 0.35% w/v in sterile isotonic phosphate buffered saline. Before release, each successive lot is tested for potency in comparison with a reference standard. Independent studies conducted by the US Public Health Service in humans have determined the amount of CT68 in stabilized solution necessary (3)(4)(5) to produce bio-equivalency with Tuberculin PPD-S (in phosphate buffer without polysorbate 80) using 5 US units (TU) Tuberculin PPD-S as the standard.
How Supplied
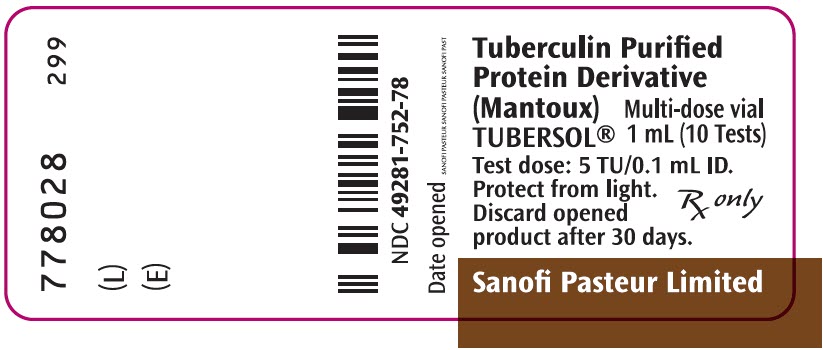
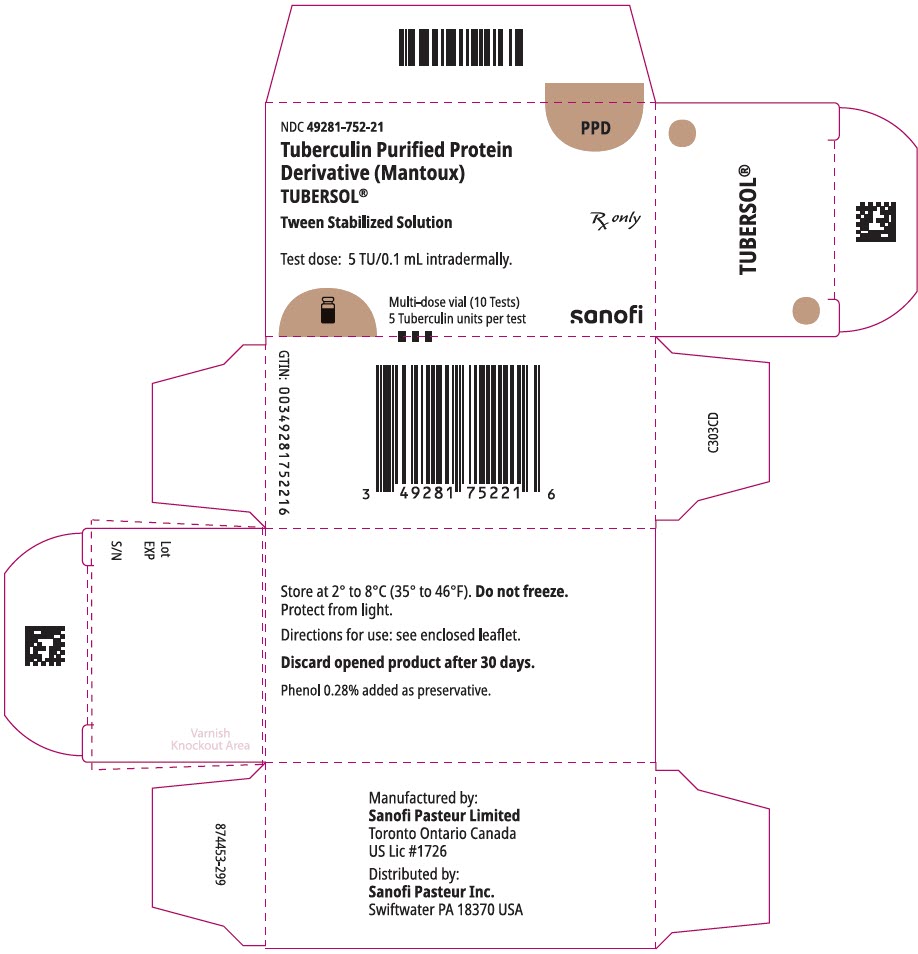
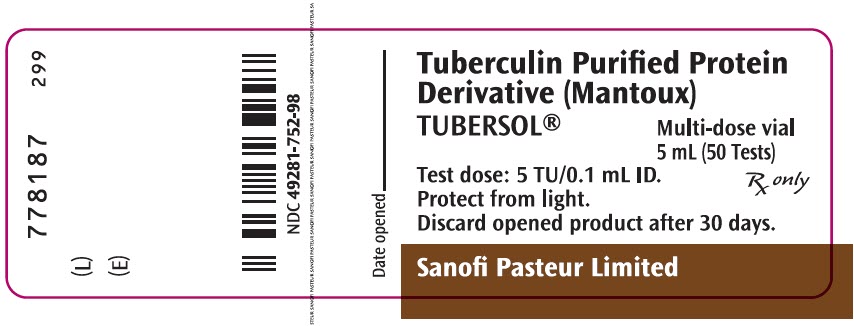
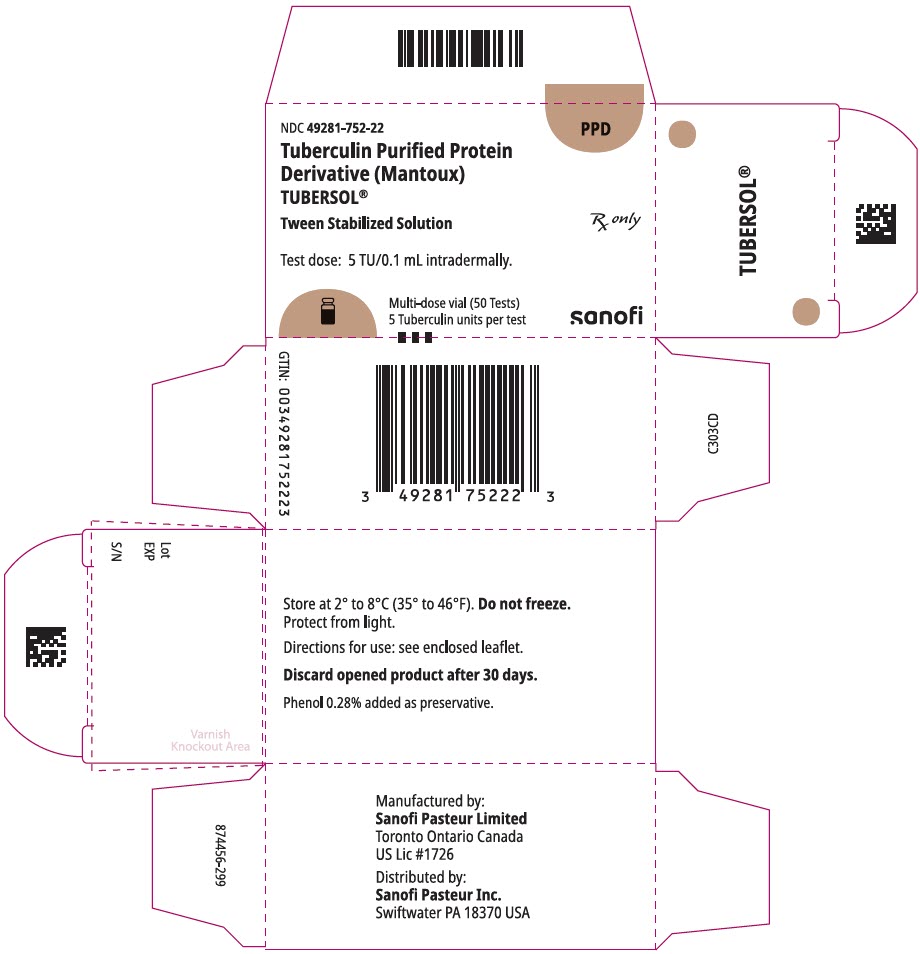
HOW SUPPLIED TUBERSOL Tuberculin Purified Protein Derivative (Mantoux), bioequivalent to 5 US units (TU) PPD-S per test dose (0.1 mL) is supplied in: 1 mL multi-dose vial (10 tests). NDC No. 49281-752-78; package of 1 vial, NDC No. 49281-752-21 5 mL multi-dose vial (50 tests). NDC No. 49281-752-98; package of 1 vial, NDC No. 49281-752-22 The stopper of the vial for this product does not contain natural latex rubber. STORAGE Store at 2° to 8°C (35° to 46°F). (19) Do not freeze. Discard product if exposed to freezing. Protect from light. Tuberculin PPD solutions can be adversely affected by exposure to light. The product should be stored in the dark except when doses are actually being withdrawn from the vial. (20) A vial of TUBERSOL which has been entered and in use for 30 days should be discarded. (21) Do not use after expiration date.
Indications & Usage
INDICATIONS AND USAGE TUBERSOL Tuberculin Purified Protein Derivative (Mantoux), is indicated to aid diagnosis of tuberculosis infection (TB) in persons at increased risk of developing active disease. The Centers for Disease Control and Prevention (CDC) have published guidelines regarding populations that would benefit from tuberculin skin testing (TST). Current recommendations can be accessed at: http://www.cdc.gov/tb/publications/factsheets/testing.htm. Previous BCG vaccination is not a contraindication to tuberculin testing. The skin-test results of BCG vaccinated persons can be used to support or exclude the diagnosis of TB infection. However, an FDA-approved interferon gamma release assay is preferred over tuberculin skin test for persons 5 years of age and older who were previously vaccinated with BCG. (8)
Dosage and Administration
DOSAGE AND ADMINISTRATION Dosage Five (5) tuberculin units (TU) per test dose of 0.1 mL is the standard strength used for intradermal (Mantoux) testing. Method of Administration TUBERSOL is indicated for intradermal injection only. Do not inject intravenously, intramuscularly, or subcutaneously . If subcutaneous injection occurs, the test cannot be interpreted. Inspect for extraneous particulate matter and/or discoloration before use. If these conditions exist, do not administer the product. Use a separate syringe and needle for each injection. (12) The following procedure is recommended for performing the Mantoux test: The preferred site of the test is the volar aspect of the forearm. Avoid areas on the skin that are red or swollen. Avoid visible veins. Clean the skin site with a suitable germicide and allow the site to dry prior to injection of the antigen. Administer the test dose (0.1 mL) of TUBERSOL with a 1 mL syringe calibrated in tenths and fitted with a short, one-quarter to one-half inch, 26 or 27 gauge needle. Wipe the stopper of the vial with a suitable germicide and allow to dry before needle insertion. Then insert the needle gently through the stopper and draw 0.1 mL of TUBERSOL into the syringe. Avoid injection of excess air with removal of each dose so as not to over pressurize the vial and possibly cause seepage at the puncture site. Insert the point of the needle into the most superficial layers of the skin with the needle bevel pointing upward and administer the dose by slow intradermal injection . If the intradermal injection is performed properly, a definite pale bleb will rise at the needle point, about 10 mm ( 3 / 8 ") in diameter. This bleb will disperse within minutes. Do not dress the site. A drop of blood may appear at the administration site following injection. Blot the site lightly to remove the blood but avoid squeezing out the injected tuberculin test fluid. In the event of an improperly performed injection (i.e., no bleb formed), repeat the test immediately at another site, at least 2 inches from the first site and circle the second injection site as an indication that this is the site to be read. Inform the patient of the need to return for the reading of the test by a trained health professional. Self-reading may be inaccurate and is strongly discouraged. Interpretation of the Test The skin test should be read by a trained health professional 48 to 72 hours after administration of TUBERSOL. Skin test sensitivity is indicated by induration only; redness should not be measured. Measure the diameter of induration transversely to the long axis of the forearm and record the measurement in millimeters (including 0 mm). (7) The tip of a ballpoint pen, gently pushed at a 45° angle toward the site of injection, will stop at the edge of induration. Also record presence and size (if present) of necrosis and edema, although these are not used in the interpretation of the test. Positive Reactions Tuberculin reactivity may indicate latent infection, prior infection and/or disease with M. tuberculosis and does not necessarily indicate the presence of active tuberculous disease. Persons showing positive tuberculin reactions should be considered positive by current public health guidelines and referred for further medical evaluation. (7)(9) The repeated testing of uninfected persons does not sensitize them to TUBERSOL. (6)(7)(9) The significance of induration measurements in diagnosing latent TB infection must be considered in terms of the patient's history and the risk of developing active TB disease as indicated in Table 1. (9) Table 1: Criteria for tuberculin positivity, by risk group Reaction ≥5 mm of Induration Reaction ≥10 mm of Induration Reaction ≥15 mm of Induration HIV-positive persons Recent contacts of tuberculosis (TB) case patients Fibrotic changes on chest radiograph consistent with prior TB Patients with organ transplants and other immunosuppressed patients (receiving the equivalent of ≥15 mg/d of prednisone for 1 month or more) Risk of TB in patients treated with corticosteroids increases with higher dose and longer duration. Recent immigrants (i.e., within the last 5 yrs) from high prevalence countries Injection drug users Residents or employees For persons who are otherwise at low risk and are tested at the start of employment, a reaction of ≥15 mm induration is considered positive. of the following high-risk congregate settings: prisons and jails, nursing homes and other long-term facilities for the elderly, hospitals and other healthcare facilities, residential facilities for patients with acquired immunodeficiency syndrome (AIDS) and homeless shelters Mycobacteriology laboratory personnel Persons with the following clinical conditions that place them at high risk: silicosis, diabetes mellitus, chronic renal failure, some hematologic disorders (e.g., leukemias and lymphomas), other specific malignancies (e.g., carcinoma of the head or neck and lung), weight loss of ≥10% of ideal body weight, gastrectomy and jejunoileal bypass Children younger than 4 yrs of age or infants, children, and adolescents exposed to adults at high-risk Persons with no risk factors for TB A TST conversion is defined as an increase of ≥10 mm of induration within a 2-year period, regardless of age. (9) The possibility should be considered that the skin test sensitivity may also be due to a previous contact with atypical mycobacteria or previous BCG vaccination. (7)(9) Negative Reactions An individual who does not show a positive reaction to 5 TU on the first test, but is suspected of being TB positive, may be retested with 5 TU. (See Booster Effect and Two-Step Testing .) Any individual who does not show a positive reaction to an initial injection of 5 TU, or a second test with 5 TU may be considered as tuberculin negative. False Positive Reactions False positive tuberculin reactions can occur in individuals who have been infected with other mycobacteria, including vaccination with BCG. (7) However, a diagnosis of M . tuberculosis infection and the use of preventive therapy should be considered for any BCG-vaccinated person who has a positive TST reaction, especially if the person has been, or is, at increased risk of acquiring TB infection. (See INDICATIONS AND USAGE .) (13)(14) False Negative Reactions Not all infected persons will have a delayed hypersensitivity reaction to a tuberculin test. In those who are elderly or those who are being tested for the first time, reactions may develop slowly and may not peak until after 72 hours. Since tuberculin sensitivity may take up to 8 weeks to develop following exposure to M. tuberculosis (see Mechanism of Action ), persons who have a negative tuberculin test <8 weeks following possible TB exposure should be retested ≥8-10 weeks following the last known or suspected exposure. (15) Altered Immune Status Impaired or attenuated cell mediated immunity (CMI) can potentially cause a false negative tuberculin reaction. Many factors have been reported to cause a decreased ability to respond to the tuberculin test in the presence of tuberculous infection including viral infections (e.g., measles, mumps, chickenpox and HIV), live virus vaccinations (e.g., measles, mumps, rubella, oral polio and yellow fever), overwhelming tuberculosis, other bacterial infections, leukemia, sarcoidosis, fungal infections, metabolic derangements, low protein states, diseases affecting lymphoid organs, drugs (corticosteroids and many other immunosuppressive agents), and malignancy or stress. (7)(16)(17) A TST should be deferred for patients with major viral infections or live-virus vaccination in the past month. Persons with the common cold may be tuberculin tested. Because TST results in HIV-infected individuals are less reliable as CD4 counts decline, screening should be completed as early as possible after HIV-infection occurs. (17) Booster Effect and Two-Step Testing If tuberculin testing will be conducted at regular intervals, for instance among healthcare workers or prison workers, two-step testing should be performed as a baseline to avoid interpreting a booster effect as a tuberculin conversion. If the first test showed either no reaction or a small reaction, the second test should be performed one to four weeks later. Both tests should be read and recorded at 48 to 72 hours. Patients with a second tuberculin test (booster) response of ≥10 mm should be considered to have experienced past TB infection. (13)(18) Persons who do not boost when given repeat tests at one week, but whose tuberculin reactions change to positive after one year, should be considered to have newly acquired tuberculosis infection and managed accordingly. (6)
