Drug Catalog - Product Detail
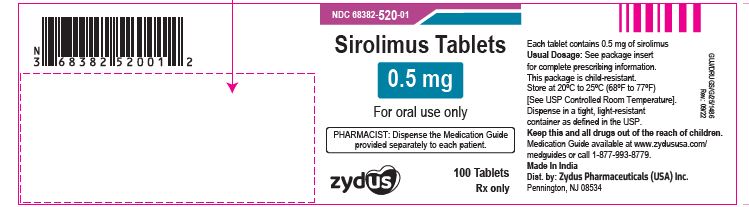
SIROLIMUS TAB 0.5 MG 100 CT
| NDC | Mfr | Size | Str | Form |
|---|---|---|---|---|
| 68382-0520-01 | ZYDUS PHARMACEUTICALS (USA) | 100 | 0.5MG | TABLET |
PACKAGE FILES
Generic Name
SIROLIMUS
Substance Name
SIROLIMUS
Product Type
HUMAN PRESCRIPTION DRUG
Route
ORAL
Application Number
ANDA201676
Description
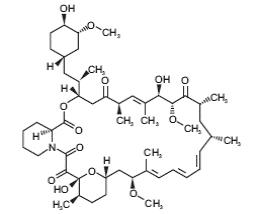
11 DESCRIPTION Sirolimus is an mTOR inhibitor immunosuppressive agent. Sirolimus is a macrocyclic lactone produced by Streptomyces hygroscopicus . The chemical name of sirolimus (also known as rapamycin) is (3 S ,6 R ,7 E ,9 R ,10 R ,12 R ,14 S ,15 E ,17 E ,19 E ,21 S ,23 S ,26 R ,27 R ,34a S )-9,10,12,13,14,21,22,23,24,25,26,27,32,33,34,34a-hexadecahydro-9,27-dihydroxy-3-[(1 R )-2-[(1 S ,3 R ,4 R )-4-hydroxy-3-methoxycyclohexyl]-1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-23,27-epoxy-3 H -pyrido[2,1-c][1,4] oxaazacyclohentriacontine-1,5,11,28,29 (4 H ,6 H ,31 H )-pentone. Its molecular formula is C 51 H 79 NO 13 and its molecular weight is 914.2. The structural formula of sirolimus is illustrated as follows. Sirolimus is a white to off-white powder and is insoluble in water, but freely soluble in benzyl alcohol, chloroform, acetone, and acetonitrile. Each sirolimus tablet intended for oral administration contains 0.5 mg or 1 mg or 2 mg of sirolimus. In addition, each tablet contains the following inactive ingredients: citric acid monohydrate, crospovidone, glyceryl monooleate, hypromellose, lactose monohydrate, microcrystalline cellulose, poloxamer, polyethylene glycol, povidone, sucrose, talc, titanium dioxide and vitamin E acetate. Additionally, each 0.5 mg tablet contains FD&C yellow #5 Aluminum Lake and iron oxide yellow and 2 mg tablet contains iron oxide black, iron oxide red and iron oxide yellow. Image
How Supplied
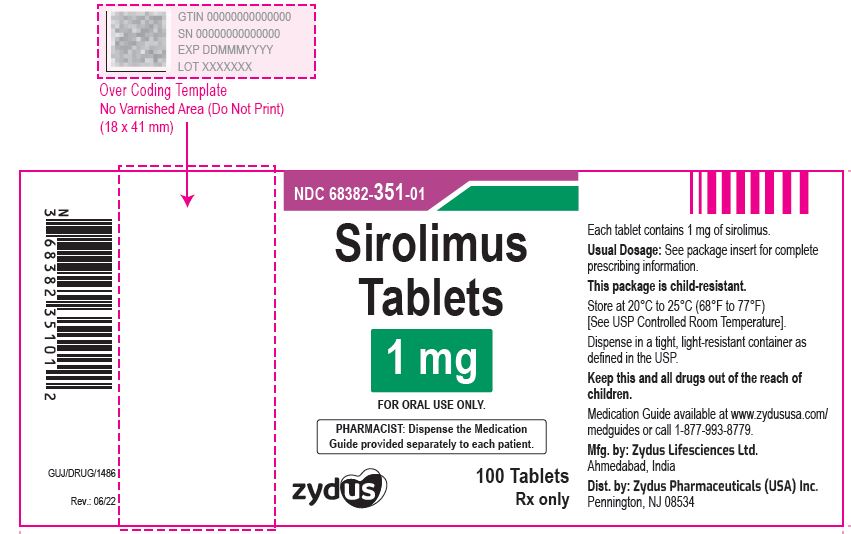
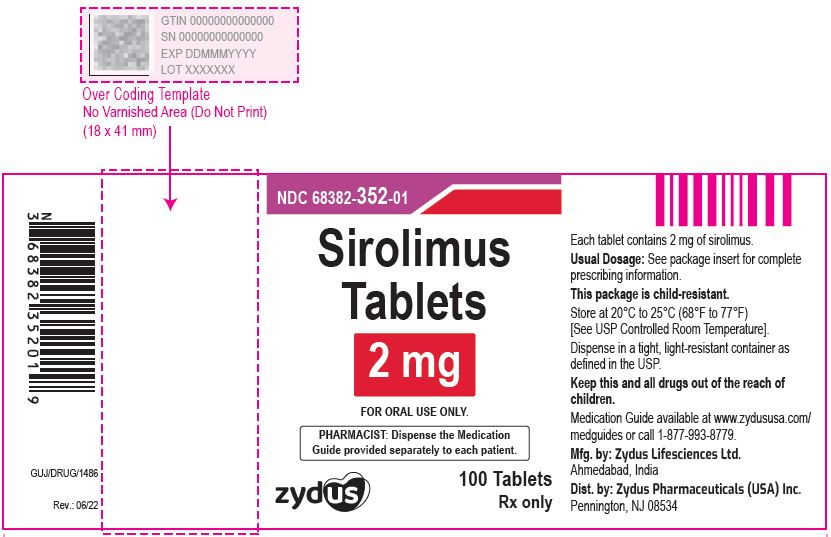
16 HOW SUPPLIED/STORAGE AND HANDLING Since sirolimus is not absorbed through the skin, there are no special precautions. However, if direct contact occurs with the skin or eyes, wash skin thoroughly with soap and water; rinse eyes with plain water. Do not use Sirolimus Tablets after the expiration date. The expiration date refers to the last day of that month. 16.2 Sirolimus Tablets Sirolimus Tablets, 0.5 mg are yellow, round, biconvex, coated tablets debossed with "1" in on one side and plain on other side and are supplied as follows: NDC 68382-520-06 in bottle of 30 tablets with child-resistant closure. NDC 68382-520-16 in bottle of 90 tablets with child-resistant closure. NDC 68382-520-01 in bottle of 100 tablets with child-resistant closure. NDC 68382-520-05 in bottle of 500 tablets NDC 68382-520-10 in bottle of 1000 tablets NDC 68382-520-77 in unit-dose blister cartons of 100 (10 x 10) unit dose tablets Sirolimus Tablets, 1 mg are white to off-white, round, biconvex, film-coated tablets debossed with 11 on one side and plain on other side and are supplied as follows: NDC 68382-351-01 in bottle of 100 tablets with child-resistant closure. NDC 68382-351-77 in unit-dose blister cartons of 100 (10 x 10) unit dose tablets Sirolimus Tablets, 2 mg are yellow, round, biconvex, coated tablets, debossed with 21 on one side and plain on other side and are supplied as follows: NDC 68382-352-01 in bottle of 100 tablets with child-resistant closure. NDC 68382-352-77 in unit-dose blister cartons of 100 (10 x 10) unit dose tablets Storage Store at 20°C to 25°C (68F° to 77°F) [See USP Controlled Room Temperature]. Use cartons to protect blister cards and strips from light. Dispense in a tight, light-resistant container as defined in the USP.
Indications & Usage
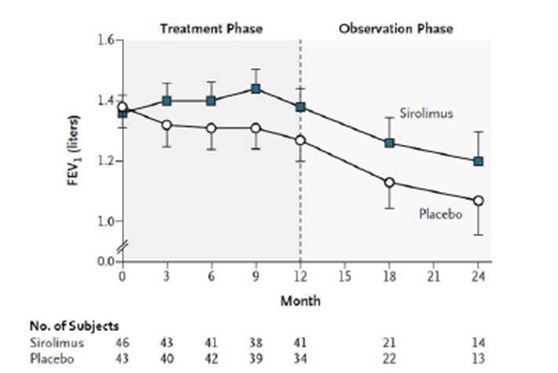
1 INDICATIONS AND USAGE Sirolimus is an mTOR inhibitor immunosuppressant indicated for the prophylaxis of organ rejection in patients aged ≥13 years receiving renal transplants: Patients at low- to moderate-immunologic risk: Use initially with cyclosporine (CsA) and corticosteroids. CsA withdrawal is recommended 2 months to 4 months after transplantation ( 1.1 ). Patients at high-immunologic risk: Use in combination with CsA and corticosteroids for the first 12 months following transplantation (1.1). Safety and efficacy of CsA withdrawal has not been established in high risk patients ( 1.1 , 1.2 , 14.3 ). Sirolimus is an mTOR inhibitor indicated for the treatment of patients with lymphangioleiomyomatosis ( 1.3 ). 1.1 Prophylaxis of Organ Rejection in Renal Transplantation Sirolimus tablets are indicated for the prophylaxis of organ rejection in patients aged 13 years or older receiving renal transplants. In patients at low- to moderate-immunologic risk, it is recommended that sirolimus tablets be used initially in a regimen with cyclosporine and corticosteroids; cyclosporine should be withdrawn 2 to 4 months after transplantation [ see Dosage and Administration ( 2.2 ) ]. In patients at high-immunologic risk (defined as Black recipients and/or repeat renal transplant recipients who lost a previous allograft for immunologic reason and/or patients with high panel-reactive antibodies [PRA; peak PRA level > 80%]), it is recommended that sirolimus tablets be used in combination with cyclosporine and corticosteroids for the first year following transplantation [ see Dosage and Administration ( 2.3 ), Clinical Studies ( 14.3 ) ]. 1.2 Limitations of Use in Renal Transplantation Cyclosporine withdrawal has not been studied in patients with Banff Grade 3 acute rejection or vascular rejection prior to cyclosporine withdrawal, those who are dialysis-dependent, those with serum creatinine > 4.5 mg/dL, Black patients, patients of multi-organ transplants, secondary transplants, or those with high levels of panel-reactive antibodies [ see Clinical Studies ( 14.2 ) ]. In patients at high-immunologic risk, the safety and efficacy of sirolimus tablets used in combination with cyclosporine and corticosteroids has not been studied beyond one year; therefore after the first 12 months following transplantation, any adjustments to the immunosuppressive regimen should be considered on the basis of the clinical status of the patient [ see Clinical Studies ( 14.3 ) ]. In pediatric patients, the safety and efficacy of sirolimus tablets have not been established in patients < 13 years old, or in pediatric (< 18 years) renal transplant patients considered at high-immunologic risk [ see Adverse Reactions ( 6.5 ), Clinical Studies ( 14.6 ) ]. The safety and efficacy of de novo use of sirolimus tablets without cyclosporine have not been established in renal transplant patients [ see Warnings and Precautions ( 5.12 ) ]. The safety and efficacy of conversion from calcineurin inhibitors to sirolimus tablet s in maintenance renal transplant patients have not been established [ see Clinical Studies ( 14.4 ) ]. 1.3 Treatment of Patients with Lymphangioleiomyomatosis Sirolimus tablets are indicated for the treatment of patients with lymphangioleiomyomatosis (LAM).
Dosage and Administration
2 DOSAGE AND ADMINISTRATION Sirolimus tablets are to be administered orally once daily, consistently with or without food [ see Dosage and Administration ( 2.5 ), Clinical Pharmacology ( 12.3 ) ]. Tablets should not be crushed, chewed or split. Patients unable to take the tablets should be prescribed the solution and instructed in its use. Renal Transplant Patients : Administer once daily by mouth, consistently with or without food ( 2 ). Administer the initial dose as soon as possible after transplantation and 4 hours after CsA ( 2.1 , 7.1 ). Adjust the sirolimus maintenance dose to achieve sirolimus trough concentrations within the target-range ( 2.5 ). Hepatic impairment: Reduce maintenance dose in patients with hepatic impairment ( 2.7 , 8.6 , 12.3 ). In renal transplant patients at low-to moderate-immunologic risk : Sirolimus and CsA Combination Therapy: One loading dose of 6 mg on day 1, followed by daily maintenance doses of 2 mg ( 2.2 ). Sirolimus Following CsA Withdrawal: 2 months to 4 months post-transplantation, withdraw CsA over 4 weeks to 8 weeks ( 2.2 ). In renal transplant patients at high-immunologic risk: Sirolimus and CsA Combination Therapy (for the first 12 months posttransplantation): One loading dose of up to 15 mg on day 1, followed by daily maintenance doses of 5 mg ( 2.3 ). Lymphangioleiomyomatosis Patients: Administer once daily by mouth, consistently with or without food ( 2 ). Recommended initial sirolimus dose is 2 mg/day ( 2.4 ). Adjust the sirolimus dose to achieve sirolimus trough concentrations between 5 to 15 ng/mL ( 2.4 ). Hepatic impairment: Reduce maintenance dose in patients with hepatic impairment ( 2.7 , 8.6 , 12.3 ). Therapeutic drug monitoring is recommended for all patients ( 2.5 , 5.17 ). 2.1 General Dosing Guidance for Renal Transplant Patients The initial dose of sirolimus tablets should be administered as soon as possible after transplantation. It is recommended that sirolimus tablets be taken 4 hours after administration of cyclosporine oral solution (MODIFIED) and or/cyclosporine capsules (MODIFIED) [ see Drug Interactions ( 7.2 ) ]. Frequent sirolimus tablets dose adjustments based on non-steady-state sirolimus concentrations can lead to overdosing or underdosing because sirolimus has a long half-life. Once sirolimus tablets maintenance dose is adjusted, patients should continue on the new maintenance dose for at least 7 to 14 days before further dosage adjustment with concentration monitoring. In most patients, dose adjustments can be based on simple proportion: new sirolimus tablets dose = current dose x (target concentration/current concentration). A loading dose should be considered in addition to a new maintenance dose when it is necessary to increase sirolimus trough concentrations: sirolimus loading dose = 3 x (new maintenance dose - current maintenance dose). The maximum sirolimus tablets dose administered on any day should not exceed 40 mg. If an estimated daily dose exceeds 40 mg due to the addition of a loading dose, the loading dose should be administered over 2 days. Sirolimus trough concentrations should be monitored at least 3 to 4 days after a loading dose(s). Two milligrams (2 mg) of Sirolimus Oral Solution have been demonstrated to be clinically equivalent to 2 mg Sirolimus Tablets; hence, at this dose these two formulations are interchangeable. However, it is not known if higher doses of Sirolimus Oral Solution are clinically equivalent to higher doses of Sirolimus Tablets on a mg-to-mg basis [ see Clinical Pharmacology ( 12.3 ) ]. 2.2 Renal Transplant Patients at Low- to Moderate-Immunologic Risk Sirolimus and Cyclosporine Combination Therapy For de novo renal transplant patients, it is recommended that sirolimus tablets be used initially in a regimen with cyclosporine and corticosteroids. A loading dose of sirolimus equivalent to 3 times the maintenance dose should be given, i.e. a daily maintenance dose of 2 mg should be preceded with a loading dose of 6 mg. Therapeutic drug monitoring should be used to maintain sirolimus drug concentrations within the target-range [ see Dosage and Administration ( 2.5 ) ]. Sirolimus Following Cyclosporine Withdrawal At 2 to 4 months following transplantation, cyclosporine should be progressively discontinued over 4 to 8 weeks, and the sirolimus dose should be adjusted to obtain sirolimus whole blood trough concentrations within the target-range [ see Dosage and Administration ( 2.5 ) ]. Because cyclosporine inhibits the metabolism and transport of sirolimus, sirolimus concentrations may decrease when cyclosporine is discontinued, unless the sirolimus dose is increased [ see Clinical Pharmacology ( 12.3 ) ]. 2.3 Renal Transplant Patients at High-Immunologic Risk In patients with high-immunologic risk, it is recommended that sirolimus be used in combination with cyclosporine and corticosteroids for the first 12 months following transplantation [ see Clinical Studies ( 14.3 ) ]. The safety and efficacy of this combination in high-immunologic risk patients has not been studied beyond the first 12 months. Therefore, after the first 12 months following transplantation, any adjustments to the immunosuppressive regimen should be considered on the basis of the clinical status of the patient. For patients receiving sirolimus with cyclosporine, sirolimus therapy should be initiated with a loading dose of up to 15 mg on day 1 post-transplantation. Beginning on day 2, an initial maintenance dose of 5 mg/day should be given. A trough level should be obtained between days 5 and 7, and the daily dose of sirolimus should thereafter be adjusted [ see Dosage and Administration ( 2.5 ) ]. The starting dose of cyclosporine should be up to 7 mg/kg/day in divided doses and the dose should subsequently be adjusted to achieve target whole blood trough concentrations [ see Dosage and Administration ( 2.5 ) ]. Prednisone should be administered at a minimum of 5 mg/day. Antibody induction therapy may be used. 2.4 Dosing in Patients with Lymphangioleiomyomatosis For patients with lymphangioleiomyomatosis, the initial sirolimus dose should be 2 mg/day. Sirolimus whole blood trough concentrations should be measured in 10 to 20 days, with dosage adjustment to maintain concentrations between 5 to 15 ng/mL [ see Dosage and Administration ( 2.5 ) ]. In most patients, dose adjustments can be based on simple proportion: new sirolimus dose = current dose x (target concentration/current concentration). Frequent sirolimus dose adjustments based on non-steady-state sirolimus concentrations can lead to overdosing or under dosing because sirolimus has a long half-life. Once sirolimus maintenance dose is adjusted, patients should continue on the new maintenance dose for at least 7 to 14 days before further dosage adjustment with concentration monitoring. Once a stable dose is achieved, therapeutic drug monitoring should be performed at least every three months. 2.5 Therapeutic Drug Monitoring Monitoring of sirolimus trough concentrations is recommended for all patients, especially in those patients likely to have altered drug metabolism, in patients ≥ 13 years who weigh less than 40 kg, in patients with hepatic impairment, when a change in the sirolimus dosage form is made, and during concurrent administration of strong CYP3A4 inducers and inhibitors [ see Warnings and Precautions ( 5.20 , 5.21 ), Drug Interactions ( 7 ) ]. Therapeutic drug monitoring should not be the sole basis for adjusting sirolimus therapy. Careful attention should be made to clinical signs/symptoms, tissue biopsy findings, and laboratory parameters. When used in combination with cyclosporine, sirolimus trough concentrations should be maintained within the target-range [ see Clinical Studies ( 14 ), Clinical Pharmacology ( 12.3 ) ]. Following cyclosporine withdrawal in transplant patients at low- to moderate-immunologic risk, the target sirolimus trough concentrations should be 16 to 24 ng/mL for the first year following transplantation. Thereafter, the target sirolimus concentrations should be 12 to 20 ng/mL. The above recommended 24 hour trough concentration ranges for sirolimus are based on chromatographic methods. Currently in clinical practice, sirolimus whole blood concentrations are being measured by both chromatographic and immunoassay methodologies. Because the measured sirolimus whole blood concentrations depend on the type of assay used, the concentrations obtained by these different methodologies are not interchangeable [ see Warnings and Precautions ( 5.17 ), Clinical Pharmacology ( 12.3 ) ]. Adjustments to the targeted range should be made according to the assay utilized to determine sirolimus trough concentrations. Since results are assay and laboratory dependent, and the results may change over time, adjustments to the targeted therapeutic range must be made with a detailed knowledge of the site-specific assay used. Therefore, communication should be maintained with the laboratory performing the assay. A discussion of different assay methods is contained in Clinical Therapeutics, Volume 22, Supplement B, April 2000 [ see References ( 15 ) ]. 2.6 Patients with Low Body Weight The initial dosage in patients ≥ 13 years who weigh less than 40 kg should be adjusted, based on body surface area, to 1 mg/m 2 /day. The loading dose should be 3 mg/m 2 . 2.7 Patients with Hepatic Impairment It is recommended that the maintenance dose of sirolimus be reduced by approximately one third in patients with mild or moderate hepatic impairment and by approximately one half in patients with severe hepatic impairment. It is not necessary to modify the sirolimus loading dose [ see Use in Specific Populations ( 8.6 ), Clinical Pharmacology ( 12.3 ) ]. 2.8 Patients with Renal Impairment Dosage adjustment is not needed in patients with impaired renal function [ see Use in Specific Populations ( 8.7 ) ].
