Drug Catalog - Product Detail
COLCHICINE 0.6MG TB 100
| NDC | Mfr | Size | Str | Form |
|---|---|---|---|---|
| 67877-0589-01 | ASCEND LABORATORIES | 100 | 0.6MG | TABLET |
PACKAGE FILES




Generic Name
COLCHICINE
Substance Name
COLCHICINE
Product Type
HUMAN PRESCRIPTION DRUG
Route
ORAL
Application Number
ANDA211250
Description
11 DESCRIPTION Colchicine is an alkaloid chemically described as (S)N-(5,6,7,9-tetrahydro-1,2,3, 10-tetramethoxy-9-oxobenzo [alpha] heptalen-7-yl) acetamide with a molecular formula of C 22 H 25 NO 6 and a molecular weight of 399.4. The structural formula of colchicine is given below. Colchicine occurs as a pale yellow powder that is soluble in water. Colchicine Tablets, USP 0.6 mg are supplied for oral administration as Purple colored, capsule shaped, film coated tablets debossed with “C6” on one side and scored on other side., containing 0.6 mg of the active ingredient colchicine, USP. Inactive ingredients: FD&C Blue #2, FD&C Red #40, hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polydextrose, polyethylene glycol, pregelatinized starch, sodium starch glycolate, titanium dioxide and triacetin. colchicine-struc
How Supplied
16 HOW SUPPLIED/STORAGE AND HANDLING 16.1 How Supplied Colchicine tablets, USP 0.6 mg are purple colored, capsule shaped, film, coated tablets debossed with “C6” on one side and scored on other side. Bottles of 30 NDC 67877-589-30 Bottles of 60 NDC 67877-589-60 Bottles of 100 NDC 67877-589-01 Bottles of 250 NDC 67877-589-86 Bottles of 500 NDC 67877-589-05 Bottles of 1000 NDC 67877-589-10 Carton of 10 (1 x 10 Unit-dose) Tablets NDC 67877-589-33 Carton of 30 (3 x 10 Unit-dose) Tablets NDC 67877-589-84 16.2 Storage Store at 20° C to 25°C (68° F to 77°F) [See USP Controlled Room Temperature]. Protect from light. DISPENSE IN TIGHT, LIGHT-RESISTANT CONTAINER.
Indications & Usage
1 INDICATIONS & USAGE Colchicine tablets are an alkaloid indicated for: Familial Mediterranean fever (FMF) in adults and children 4 years or older ( 1.2 ). 1.2 Familial Mediterranean Fever (FMF) Colchicine tablets are indicated in adults and children four years or older for treatment of familial Mediterranean fever (FMF).
Dosage and Administration
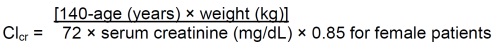
2 DOSAGE & ADMINISTRATION The long-term use of colchicine is established for FMF. The recommended dosage of colchicine tablets depends on the patient’s age, renal function, hepatic function and use of coadministered drugs [see Dosage and Administration ( 2.4 , 2.5 , 2.6 )]. Colchicine tablets are administered orally without regard to meals. Colchicine tablets are not an analgesic medication and should not be used to treat pain from other causes. FMF: Adults and children older than 12 years 1.2 – 2.4 mg; children 6 to 12 years 0.9 – 1.8 mg; children 4 to 6 years 0.3 – 1.8 mg ( 2.2 , 2.3 ). Give total daily dose in one or two divided doses ( 2.2 ). Increase or decrease the dose as indicated and as tolerated in increments of 0.3 mg/day, not to exceed the maximum recommended daily dose ( 2.2 ). Colchicine tablets are administered orally without regard to meals. See full prescribing information (FPI) for dose adjustment regarding patients with impaired renal function ( 2.5 ), impaired hepatic function ( 2.6 ), the patient’s age ( 2.3 , 8.5 ) or use of coadministered drugs ( 2.4 ). 2.2 FMF The recommended dosage of colchicine tablets for FMF in adults is 1.2 mg to 2.4 mg daily. Colchicine tablets should be increased as needed to control disease and as tolerated in increments of 0.3 mg/day to a maximum recommended daily dose. If intolerable side effects develop, the dose should be decreased in increments of 0.3 mg/day. The total daily colchicine tablets dose may be administered in one to two divided doses. 2.3 Recommended Pediatric Dosage FMF The recommended dosage of colchicine tablets for FMF in pediatric patients 4 years of age and older is based on age. The following daily doses may be given as a single or divided dose twice daily: Children 4 to 6 years: 0.3 mg to 1.8 mg daily Children 6 to 12 years: 0.9 mg to 1.8 mg daily Adolescents older than 12 years: 1.2 mg to 2.4 mg daily 2.4 Dose Modification for Coadministration of Interacting Drugs Concomitant Therapy Coadministration of colchicine tablets with drugs known to inhibit CYP3A4 and/or P-glycoprotein (P-gp) increases the risk of colchicine-induced toxic effects (Table 1) . If patients are taking or have recently completed treatment with drugs listed in Table 1 within the prior 14 days, the dose adjustments are as shown in the table below [see Drug Interactions ( 7 )]. Table 1. Colchicine tablets Dose Adjustment for Coadministration with Interacting Drugs if No Alternative Available* Strong CYP3A4 Inhibitors † Drug Noted or Anticipated Outcome FMF Original Intended Dosage Adjusted Dose Atazanavir Clarithromycin Darunavir/ Ritonavir ‡ Indinavir Itraconazole Ketoconazole Lopinavir/ Ritonavir ‡ Nefazodone Nelfinavir Ritonavir Saquinavir Telithromycin Tipranavir/Ritonavir ‡ Significant increase in colchicine plasma levels*; fatal colchicine toxicity has been reported with clarithromycin, a strong CYP3A4 inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other strong CYP3A4 inhibitors. Maximum daily dose of 1.2 – 2.4 mg Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Moderate CYP3A4 Inhibitors FMF Drug Noted or Anticipated Outcome Original Intended Dosage Adjusted Dose Amprenavir ‡ Aprepitant Diltiazem Erythromycin Fluconazole Fosamprenavir ‡ (prodrug of Amprenavir) Grapefruit juice Verapamil Significant increase in colchicine plasma concentration is anticipated. Neuromuscular toxicity has been reported with diltiazem and verapamil interactions. Maximum daily dose of 1.2 – 2.4 mg Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day) P-gp Inhibitors † FMF Drug Noted or Anticipated Outcome Original Intended Dosage Adjusted Dose Cyclosporine Ranolazine Significant increase in colchicine plasma levels*; fatal colchicine toxicity has been reported with cyclosporine, a P-gp inhibitor. Similarly, significant increase in colchicine plasma levels is anticipated with other P-gp inhibitors. Maximum daily dose of 1.2 –2.4 mg Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) * For magnitude of effect on colchicine plasma concentrations [see Clinical Pharmacology ( 12.3 )] † Patients with renal or hepatic impairment should not be given colchicine tablets in conjunction with strong CYP3A4 or P-gp inhibitors [see Contraindications ( 4 )] ‡ When used in combination with Ritonavir, see dosing recommendations for strong CYP3A4 inhibitors [see Contraindications ( 4 )] Table 2. Colchicine tablets Dose Adjustment for Coadministration with Protease Inhibitors Protease Inhibitor Clinical Comment w/Colchicine-Treatment of FMF Atazanavir sulfate (Reyataz) Patients with renal or hepatic impairment should not be given colchicine with Reyataz. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Darunavir (Prezista) Patients with renal or hepatic impairment should not be given colchicine with Prezista/ ritonavir. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Fosamprenavir (Lexiva) with Ritonavir Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Fosamprenavir (Lexiva) Patients with renal or hepatic impairment should not be given colchicine with Lexiva/ritonavir. Maximum daily dose of 1.2 mg (may be given as 0.6 mg twice a day) Indinavir (Crixivan) Patients with renal or hepatic impairment should not be given colchicine with Crixivan. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Lopinavir/ Ritonavir (Kaletra) Patients with renal or hepatic impairment should not be given colchicine with Kaletra. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Nelfinavir mesylate (Viracept) Patients with renal or hepatic impairment should not be given colchicine with Viracept. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Ritonavir (Norvir) Patients with renal or hepatic impairment should not be given colchicine with Norvir. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Saquinavir mesylate (Invirase) Patients with renal or hepatic impairment should not be given colchicine with Invirase/ ritonavir. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) Tipranavir (Aptivus) Patients with renal or hepatic impairment should not be given colchicine with Aptivus/ritonavir. Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day) 2.5 Dose Modification in Renal Impairment Colchicine dosing must be individualized according to the patient's renal function [see Use in Specific Populations ( 8.6 )]. Clcr in mL/minute may be estimated from serum creatinine (mg/dL) determination using the following formula: FMF Caution should be taken in dosing patients with moderate and severe renal impairment and in patients undergoing dialysis. For these patients, the dosage should be reduced [see Clinical Pharmacology ( 12.3 )]. Patients with mild (Clcr 50 to 80 mL/min) and moderate (Clcr 30 to 50 mL/min) renal impairment should be monitored closely for adverse effects of colchicine tablets. Dose reduction may be necessary. For patients with severe renal failure (Clcr less than 30 mL/min), start with 0.3 mg/day; any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine [see Use in Specific Populations ( 8.6 )]. For patients undergoing dialysis, the total recommended starting dose should be 0.3 mg (half tablet) per day. Dosing can be increased with close monitoring. Any increase in dose should be done with adequate monitoring of the patient for adverse effects of colchicine [see Clinical Pharmacology ( 12.3 ), Use in Specific Populations ( 8.6 )]. colchicine-formula 2.6 Dose Modification in Hepatic Impairment FMF Patients with mild to moderate hepatic impairment should be monitored closely for adverse effects of colchicine. Dose reduction should be considered in patients with severe hepatic impairment [see Use in Specific Populations ( 8.7 )].
